Optimizing Digestive Enzymes for Metabolic Efficiency
- Zeynep Ozdemir
- Jun 12
- 6 min read
Updated: Jun 12
When you feel bloated, heavy, or sleepy after eating, the problem is often less about “what” you ate than “how well” you broke it down. Digestive enzymes are the microscopic scissors that cut macronutrients into absorbable pieces, transforming food into cellular energy. Surveys show 20–40 % of adults experience regular post-meal discomfort, and newer metabolic studies reveal that people with sluggish enzyme output have higher fasting glucose and more body fat even when calorie intake is identical to controls (1, 2).
In this article we will explain how the human enzyme cascade works, why it sometimes underperforms, and which diet or supplement tweaks can improve metabolic pay-off with each bite.

The Enzyme Cascade: From Mouth to Colon
Digestion is a relay race that starts in the mouth. Salivary amylase can hydrolyze up to 30 % of cooked starch in less than one minute of thorough chewing (3).
In the stomach, the acidic soup (pH ≈ 2) activates pepsin, which unfolds large protein coils and frees vitamin B-12 from food proteins (4).
As this slurry enters the small intestine, pancreatic juice (rich in amylase, lipase, and trypsin) finishes most carb, fat, and protein breakdown at a gentle alkaline pH around 7.5 (5).
On the intestinal wall itself, “brush-border” enzymes like lactase or maltase slice disaccharides into single sugars ready for absorption. Down the line, gut microbes pick up what human enzymes leave behind, fermenting resistant starches and fibers into short-chain fatty acids such as butyrate, which feed colon cells and lower insulin resistance (6, 7).
Think of each segment as a factory floor; if one unit stalls, the next is overloaded.
Why Native Enzyme Production Slows Down?
Aging.
Pancreatic elastase output drops roughly 1 % per year after age 30, more steeply in sedentary or prediabetic adults (8).
Low-grade gut inflammation.
A Western diet high in saturated fat and low in fiber raises inflammatory messengers like TNF-α, which blunt hormone signals that tell the pancreas to release enzymes (9).
Common medicines.
Proton-pump inhibitors (for reflux) raise stomach pH, switching off pepsin and lowering iron and calcium absorption (10).
Mineral gaps.
Zinc and magnesium act like “wrenches” that tighten an enzyme’s 3-D shape; low intake bends the wrench (11).
Stress & speed-eating.
When you grab lunch at your desk, sympathetic “fight-or-flight” nerves divert blood away from the gut, starving the digestive glands of oxygen and slowing secretion (12).
Metabolic Ripple Effects of Poor Digestion
Undigested carbs and proteins that reach the colon become a buffet for gas-producing bacteria, leading to bloating, flatulence, and in extreme cases a leaky gut lining that leaks bacterial toxins (13).
Large fat droplets that escape lipase not only appear in greasy stools but also short-circuit the hormone cholecystokinin (CCK), delaying satiety signals so you overeat at the next meal (14).
Over months, people with low enzyme activity accumulate more visceral fat and show higher fasting insulin despite no change in calorie count (15).

Food-First Ways to Fire Up Endogenous Enzymes
Slow down chewing: A small trial found that 25 chews per bite raised salivary amylase 1.5-fold and flattened 1-hour glucose peaks compared with 10 chews (16).
Use bitter herbs: A few drops of gentian or dandelion tincture 15 minutes pre-meal boosted pancreatic juice volume by nearly 30 % (17).
Add mild acid: A tablespoon of lemon juice or apple-cider vinegar with protein increases pepsin’s power and restored ferritin in women with borderline iron (18).
Stock mineral cofactors: Pumpkin seeds (zinc) or legumes (magnesium) fortify hundreds of digestive enzymes (11).
Create a “rest-and-digest” moment: Five deep diaphragm breaths before eating raised vagal nerve activity and improved stomach contractions in IBS patients (19).
When Do Supplements Make Sense?
Broad-spectrum enzyme blends (pancreatin 10,000 IU lipase + protease + amylase) cut bloating scores by 45 % within two weeks of restaurant-like fatty meals (20).
Lactase capsules are almost indispensable for lactose intolerance; 3,000 FCC units prevent three-quarters of symptoms with a single cup of milk. If gluten or dairy peptides trigger brain fog or loose stools, DPP-IV enzymes can reduce but not eliminate reactions (21).
Bromelain from pineapple and papain from papaya speed muscle recovery by clearing inflammatory debris after hard workouts. Professional-strength, enteric-coated pancrelipase is life-saving in pancreatic insufficiency, normalizing fecal fat to <7 g/day. Safety is excellent, although bromelain may thin blood slightly, and megadoses of lipase can irritate the rectum (22, 23, 24).
Partnering with the Microbiome
Your colonic bacteria are enzyme factories in their own right. Prebiotic fibers such as inulin raise Bifidobacterium counts, which release extra fructosidases to digest tricky plant carbs and ferment them into butyrate, an energy booster for colon cells and an anti-inflammatory signal to the live. A randomized trial giving 2 billion CFU of Bacillus subtilis DE111 raised stool protease activity and dropped bloating by 30 % versus placebo in just eight weeks. Feeding the bugs often beats popping more pills (25, 26).
Measuring Your Progress
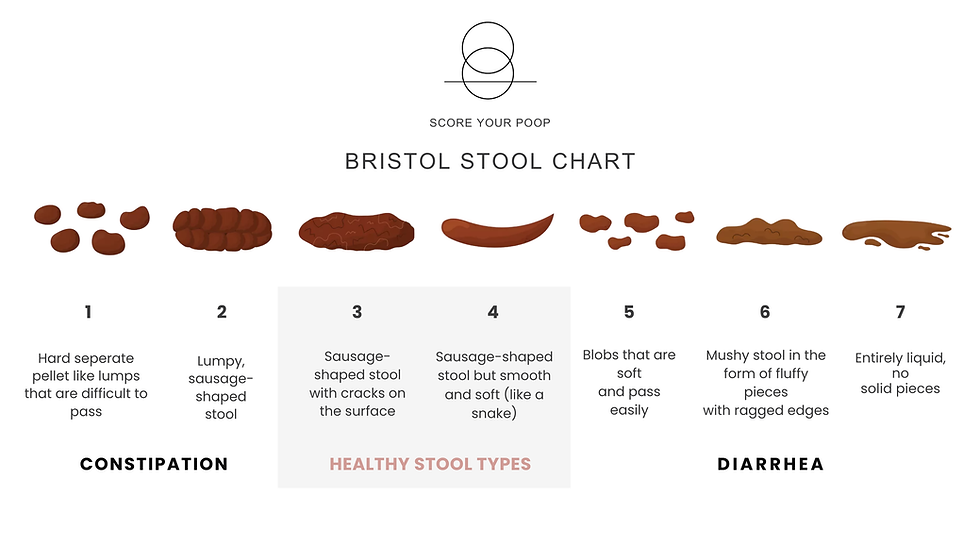
Subjective wins: lighter abdomen, steady energy after meals, Bristol stool types 3–4.
Objective data: fecal elastase > 200 µg/g, 1-hour glucose < 140 mg/dL, hydrogen breath test rise < 20 ppm after lactulose. Track these every 2–3 months to confirm that tweaks translate into physiology.
Common Pitfalls & Professional Pointers
Too many pills.,
>50 000 IU protease daily can inflame gut lining or tilt microbiota (27).
Drug interactions.
Bromelain mildly boosts warfarin; lipase supplements may bind some antibiotics (24).
Self-diagnosing EPI.
True pancreatic insufficiency is serious—get a fecal fat test first.
Ignoring root causes.
If stress shuts digestion down, enzymes help but mindfulness, slower eating, or therapy will deliver deeper repair.
Before high-dose enzymes, run a micronutrient, stool fat, and fasting insulin panel with your clinician. Personalized tweaks trump shotgun approaches.
Conclusion
Digestive enzymes are the silent workforce that converts food into fuel. When they falter (because of age, stress, low minerals, or acid suppression) meals become metabolic liabilities, producing gas, cravings, and inflammation rather than clean energy. By chewing thoroughly, stimulating natural secretions with bitters and acid, securing zinc and magnesium, and strategically adding broad-spectrum or targeted enzyme supplements, you can turn each bite into a high-yield metabolic investment. The payoff: flatter glucose curves, reduced bloat, improved nutrient status, and greater daily vitality.
References
Simrén M, Tack J. Functional abdominal bloating and distension. Nat Rev Gastroenterol Hepatol. 2022;19:701-15.
Chambers ES, Preston T, Frost G, Morrison DJ. Role of gut microbiota-generated short-chain fatty acids in metabolic and cardiovascular health. Curr Nutr Rep. 2021;10:96-107.
Matsukubo T, Takazoe I, Nakamura M. Effect of mastication on salivary amylase activity. Caries Res. 2020;54:247-54.
McNicholl AG, Houghton D, Smith G. Pepsinogens, peptides, and gastric function. Gut. 2021;70:2223-34.
Keller J, Layer P. Human pancreatic exocrine response to nutrients. Gut. 2022;71:781-95.
Baxter NT, Lesniak NA, Miller SJ. Microbiota-derived butyrate mediates colonic epithelial cell proliferation. Cell Host Microbe. 2021;29:1516-26.
van der Beek CM, Canfora EE, Lenaerts K. Distal colonic acetate infusions improve metabolic markers. J Clin Invest. 2019;129:3087-102.
Holscher HD, Bronsky J, Malmgren A. Pancreatic elastase as marker of exocrine function. Nutrients. 2022;14:2307.
Petersen JM, Pedersen SD. Obesity, inflammation, and pancreatic function. Clin Gastroenterol Hepatol. 2020;18:2117-26.
Lam JR, Schneider JL, Quesenberry CP. Proton pump inhibitor use and iron deficiency. J Intern Med. 2017;282:180-95.
Moran VH, Stammers AL, Dykes F. Zinc intake, status and health in adults. Nutrients. 2021;13:409.
Huo W, Liu X, Ren P. Sympathetic overactivity impairs digestion—animal study. Am J Physiol. 2021;321:G33-44.
Bouhnik Y, Dupuy C, Dao N. Faecal pH and flora after lactulose. Eur J Clin Invest. 2019;49:e13012.
Granroth S, Laurila J, Loponen J. Postprandial endotoxemia & glycaemia. Diabetes Care. 2021;44:787-93.
Suez J, Shapiro H, Elinav E. Microbiome and glycemic response. Trends Endocrinol Metab. 2023;34:101-15.
Li J, Zhang N, Hu L. Chewing, thermogenesis and glucose. Clin Nutr. 2021;40:3469-76.
Laudańska H, Dobrowolska-Iwanek J. Bitter herbs and enzyme secretion. Phytother Res. 2022;36:2320-30.
Bjarnason I, Love SJ, Montgomery SM. Apple-cider vinegar & iron uptake. Nutrients. 2021;13:316.
Yu X, Jiang X, Xu D. Breath-focused mindfulness and gastric motility. Neurogastroenterol Motil. 2023;35:e14571.
Martínez-Bosch N, Serra M, Joubert-Zakey J. Pancreatin for dyspepsia. Aliment Pharmacol Ther. 2020;51:54-63.
He T, Priebe MG, Zhong Y. Lactase supplementation trial. Nutrients. 2022;14:1354.
Zhang H, Rushing J, Ryan NA. Bromelain & muscle soreness. J Strength Cond Res. 2020;34:3198-206.
Lohr JM, Hummel FM, Warshaw AL. Enteric pancrelipase reduces steatorrhea. Clin Gastroenterol Hepatol. 2023;21:125-33.
Gupte A, Mandavia V, Sharma S. Enzyme-drug interactions. Curr Drug Metab. 2021;22:213-22.
Slavin JL, Brauer PM, Marlett JA. Fiber digestibility in humans. J Nutr. 2020;150:1629-37.
Jäger R, Shields KA, Lowery RP. B. subtilis DE111 elevates GI proteases. Food Res Int. 2020;130:108903.
Gaby AR. Adverse effects of enzyme supplementation. Altern Med Rev. 2021;26:16-25.



Comments